DISCOVER
Thinking Healthy Program – Preschool
Brief background & description
High prevalence and recurrence of perinatal depression in developing countries indicates the need for longer-term evidence-based interventions with a life course approach to address this burden and to minimize its adverse consequences for both the mother and her child’s developmental outcomes including mortality and morbidity[1-3].
In Pakistan, a Cognitive Behaviour Therapy (CBT) based psycho-social intervention for perinatal depression called the Thinking Healthy Programme (THP), more than halved the rates of perinatal depression, in the first year postnatal, in rural settings [4]; THP has also been taken up by WHO in 2015 as part of their series of low-intensity psychosocial interventions for global dissemination[5]. The THP was an early intervention starting in pregnancy and going through to first year postnatal; THP was task-shifted and delivered through Lady Health Workers (LHWs). Owing to community workers being overburdened which is a barrier to scale-up, we adapted THP for delivery through lay peers (other mothers in the same communities) which was found to be effective in reducing depression in the first 3 months postnatal and overall helped sustained recovery over the six months postnatal [6, 7]. This too being an early intervention, called Thinking Healthy Program Peer-delivered (THPP), lasted up to the 5th month postnatal (with 14 sessions in all). In light of recent evidence from Pakistan warrants longer-term interventions to help promote wellbeing and prevent recurrence of maternal depression along with promoting early childhood development [8]. In view of this, THPP was extended to continue beyond the 5th month postnatal through to 3 years postnatal (with 18 group sessions in all); adding early childhood development appropriate content, we called it the Thinking Healthy Program Peer-delivered Plus (THPP+) and is being tested for its effectiveness [9].
Now THPP+ is nearing its culmination at 3 years of child’s age but provides a unique opportunity to convert it into a life course approach intervention by extending it into preschool age of the child. We extended THPP+ for another two years and are calling this component as the “THP Preschool”. This will help promote school readiness among children by their 5th year of life apart from focusing on participant mothers’ continued wellbeing.
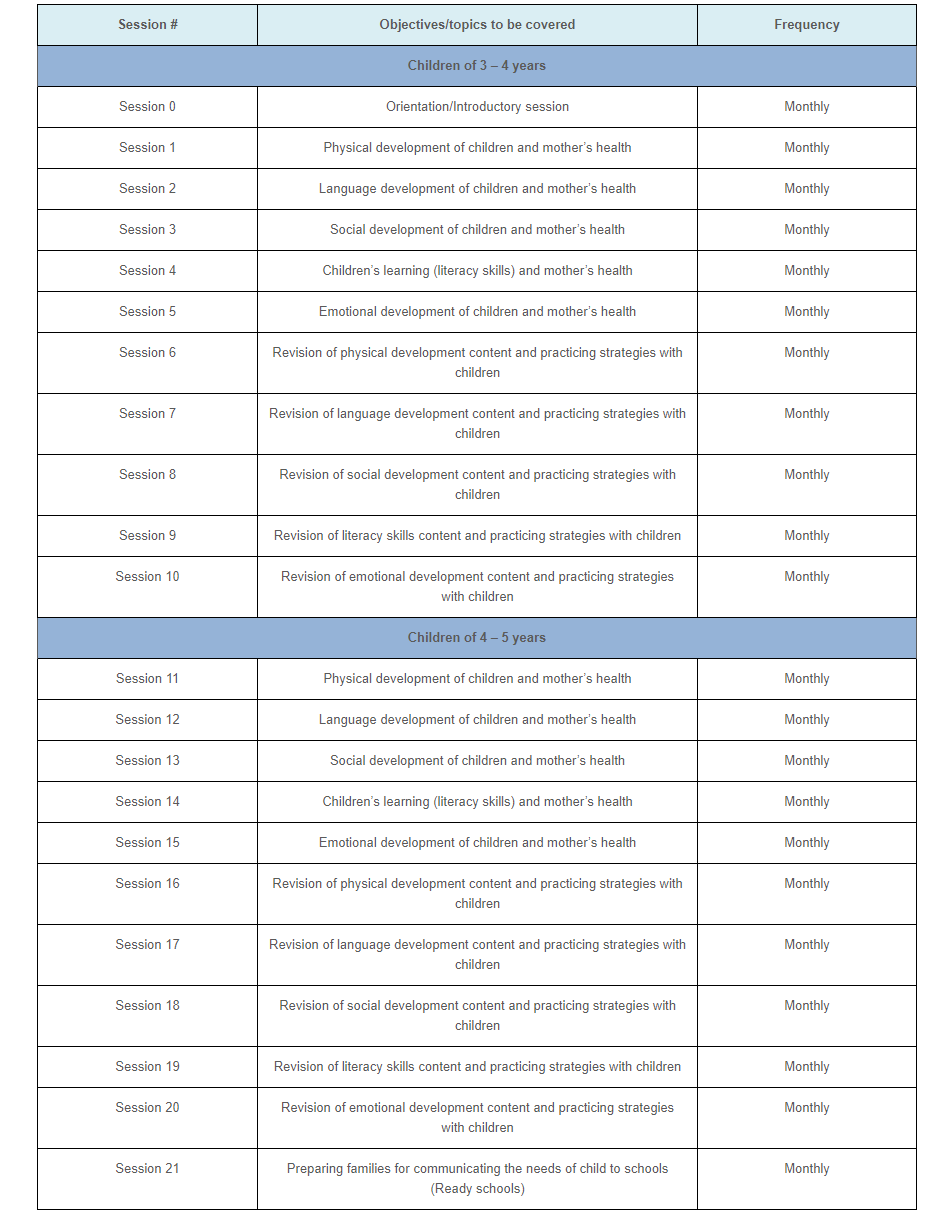
School readiness, if promoted helps learning at school as well as helping the child staying in school. UNICEF describes school readiness to have three main dimensions; i.e. children’s readiness for schools, schools’ readiness for children and families’ and communities’ readiness for schools[10]. School readiness content within the THP-Preschool (THP-PS) has been informed by an evidence based intervention called Learning Through Play[11]. It includes 5 key domains at children’s level a) physical wellbeing and motor development b) language development c) social development d) literacy and cognitive skills e) emotional development; along with maternal wellbeing as the 6th domain. THP-PS will be delivered by the same trained peers (other mothers) that have been delivering THPP and THPP+ and in partnership with the community health workers ie LHWs. THP-PS sessions start from the 3rd year of child’s age and continue through to the 5th year. The intervention will be delivered through 21 home based individual face to face sessions. Details of the timing, content and frequency is given in the table below.
Thinking Healthy Program – Preschool Sessions
References
- Weobong, B., et al., Association between probable postnatal depression and increased infant mortality and morbidity: findings from the DON population-based cohort study in rural Ghana. BMJ Open, 2015 5(8).
- Weobong, B., et al., Association of antenatal depression with adverse consequences for the mother and newborn in rural Ghana: findings from the DON population-based cohort study. PLoS One. , 2014. 9(12).
- Chen, Y.H., S.Y. Tsai, and H.C. Lin, Increased mortality risk among offspring of mothers with postnatal depression: a nationwide population-based study in Taiwan. Psychol Med, 2011 41(11).
- Rahman, A., et al., Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet, 2008. 372(9642): p. 902-9.
- World Health Organization. Thinking Healthy: A Manual for Psychosocial Management of Perinatal Depression (WHO generic field-trial version 1.0). Geneva, WHO,, 2015.
- Atif, N., et al., Mother-to-mother therapy in India and Pakistan: adaptation and feasibility evaluation of the peer-delivered Thinking Healthy Programme. BMC Psychiatry, 2017. 17(1): p. 017-1244.
- Sikander, S., et al., Delivering the Thinking Healthy Programme for perinatal depression through volunteer peers: a cluster randomised controlled trial in Pakistan Lancet Psychiatry, 2019. 6(2): p. 128-139.
- Maselko, J., et al., Effect of an early perinatal depression intervention on long-term child development outcomes: follow-up of the Thinking Healthy Programme randomised controlled trial. Lancet Psychiatry, 2015. 2(7): p. 609-17.
- Turner, E.L., et al., The effectiveness of the peer-delivered Thinking Healthy PLUS (THPP+) Program for maternal depression and child socioemotional development in Pakistan: study protocol for a randomized controlled trial. Trials, 2016. 17(1): p. 016-1530.
- United Nations Children’s Fund (UNICEF), School readiness: A conceptual framework. 2012: New York.
- Rahman, A., et al., Cluster randomized trial of a parent-based intervention to support early development of children in a low-income country. Child Care Health Dev, 2009. 35(1): p. 56-62.